Eswatini has made major investments in improving malaria control and surveillance, including significant policy changes enabling the NMP to rapidly respond to cases. Despite all the efforts to make Eswatini malaria-free by 2020, there has been little change over the past decade and the overall elimination strategy has fallen short of its target. Eswatini has managed to keep malaria controlled, with relatively low annual incidence rates compared to its neighbour Mozambique and other E-2020 countries in the region [1, 22]. However, outbreaks could still not be prevented within the case study’s observation period. The reviewed data suggests that higher case numbers are associated with decreased vector control efforts. This is especially well illustrated in 2017 when hardly any structures were sprayed, and local malaria transmission increased rapidly, reaching an unprecedented high over the study observation period. Whilst a surveillance system has been established in the country, the epidemiological case investigation rate is only 84%, with around a fifth of the reported cases remaining uninvestigated. Case classification is based on 3 categories (autochthonous, imported, and unknown), leaving out introduced cases, which are an important marker of local transmission. This must be improved if elimination is to be achieved. Reviewing the NMP databases highlighted significant missing demographic data (GPS coordinates, case origin data) that limited the mapping of malaria cases and IRS coverage. This missing information is pertinent for a country that is aiming for elimination, as all cases need to be identified and mapped for proper and effective deployment of vector control interventions [20].
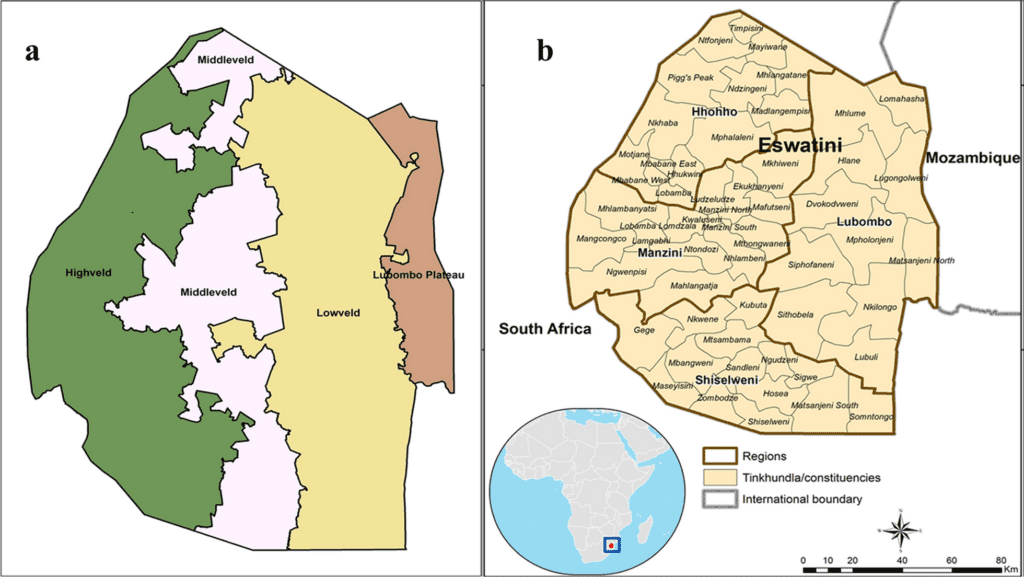
IRS remains one of the most powerful vector control interventions for reducing/interrupting malaria transmission in terms of its immediate impact. Its use in the last seven decades has played a major role in the elimination of malaria from southern Europe, the Mediterranean region, Russia, large parts of Asia and Latin America, as well as many parts of South Africa [23]. In Eswatini, IRS is supposed to be implemented annually in October, marking one spray cycle before the start of the major local malaria season. This strategy is based on malaria transmission occurring during the warmer and wetter months of November to April. Also, this strategy targets the local cases that seem to peak later in the year as observed in this case study, marking the duration of the transmission season of November–April. The frequency of IRS application depends on, among other factors, the insecticide used and the structure types. Eswatini sprayed DDT in mud structures and pyrethroids in modern/cement structures due to a difference in the residual effect of each insecticide on different wall types. In 2016, the IRS effort was reduced and targeted at the few local transmission hotspots observed in the previous year when IRS was more widely applied. In 2017, hardly any IRS was done. This reduced vector control effort correlated with major outbreaks of local cases in an expanded area of lowveld and lower middleveld regions. The exploration of the data suggests that IRS applications were frequently targeted in areas seen to be persistent malaria hotspots in the previous year. However, this targeted approach might have not considered that the higher coverage with IRS in the previous year prevented most of the cases that would have been seen without intervention. The increase of the IRS efforts in 2018 was associated with reductions in malaria incidence.
The mapped locations receiving IRS from the data provided by the NMP surveillance highlights significant gaps in the strategic deployment of this vector control tool to targeted malaria hotspots in part of the studied period (years). Studies have shown IRS to be an effective strategy for preventing malaria infection and mortality across a range of transmission settings [24,25,26,27,28,29]. However, low coverage and poor quality of IRS can limit the impact on malaria transmission [29]. Eswatini’s low coverage in 2017 was attributed to challenges in the procurement of insecticide, hence only limited amounts of insecticide (lambda-cyhalothrin) that remained from the previous season were used and targeted at outbreaks rather than prior transmission season hotspots. In 2018, IRS coverage maps show much more spraying. However, the challenges in procurement extended to 2018 and hence whilst there was increased coverage, the timing of IRS was not adhered to and was done late in many targeted regions [14]. In summary, the challenges experienced by the NMP are due to procurement and resource allocation, which led to poor planning and execution of IRS and thus, insufficient coverage. Since IRS is at the core of Eswatini’s vector control strategy, this delay had a major impact on malaria control. To get on track with the elimination effort, the NMP must identify and address the challenges in the implementation of IRS to sustain vector control. Clearly, in Eswatini, logistics is the main challenge in implementing a timely and effective IRS.
Many factors have been shown to contribute to malaria outbreaks in various settings in Eswatini, including rainfall, temperature, population movement, and the lack of sufficient or appropriate control tools or timings of vector control strategies [18]. Control of malaria transmission in border areas, together with the importation of cases, presents a major threat to successfully eliminating malaria in Eswatini. Population movement, especially from the malaria-endemic neighbouring Mozambique, has been previously recorded as an important factor contributing to the persistence of malaria cases in Eswatini [30]. The reviewed data supported these international border movements contributing to malaria cases.
Eswatini can be described as a low-transmission and high-importation case, similar to what was described in a study of Ethiopia, where the local transmission risk was very low, but many cases likely originated from other countries [31]. The high numbers of imported cases that were observed in this Eswatini study during the first few months of the year were likely caused by workers from Mozambique returning to Eswatini in January following the Christmas and New Year holidays [30]. A study conducted in 2016 on travel patterns and demographic characteristics of malaria cases in Eswatini attributed high malaria case importation rates to sugar plantation workers, whose travel patterns are well known between these two countries [30]. Furthermore, the study reported that, since international travellers tend to spend more time away than domestic travellers, they are at a higher risk of getting malaria, especially those travelling to malaria-endemic areas. This length of stay increases the risks of acquiring and returning with parasites. Also, adolescents and employed males were showed to be frequent travellers [30].
Currently, Eswatini’s NMP carries out malaria screening at the Eswatini/Mozambique border, where they do not treat the positive cases but rather refer them to the nearest health facility. The data in this study indicate that outbreaks are due to local transmission, which calls for two different responses: for cases imported to areas where transmission is unlikely, it is more a medical treatment case, so there should be border checks and treatment; whilst for local cases, there needs to be more emphasis on vector control. Elsewhere, it has been previously demonstrated in Eastern Myanmar that early diagnosis and prompt onsite treatment of confirmed cases is effective in achieving malaria elimination [32]. Also, it has been observed in southern Iran that the presence of foreign immigrants could cause malaria outbreaks [33]. Cross-border malaria control initiatives are important in supporting malaria elimination efforts, especially when low-transmission countries share borders with higher-transmission countries. Therefore, there is a need for Eswatini to strengthen its cross-border surveillance, form collaborations with its neighbouring countries, and learn from past lessons such as the cross-border initiative Lubombo Spatial Development Initiative (LSDI) [6]. This initiative represented collaborative efforts between Eswatini, Mozambique and South Africa to reduce each country’s malaria importation risk and achieve elimination. LSDI led to success towards malaria elimination in both South Africa and Eswatini, with IRS as the core intervention [6, 7]. However, the termination of LSDI resulted in an upsurge of malaria cases in these countries, mainly as a result of migration from high-transmission areas to low-transmission ones [6]. The LSDI focus on vector control with IRS further demonstrates the important role of vector control in elimination efforts, and in particular, IRS.
In recent years, Eswatini has engaged in cross-border collaborations with the neighbouring countries of Mozambique and South Africa [14] and regional collaborations via the E-8 initiative [3] as well as partnering with development partners in efforts to tackle cross-border malaria transmission and to augment national efforts towards elimination. The E-8’s mandate has a particular focus on Migrants and Mobile Populations (MMPs) where Eswatini is a recipient of funds through the Initiative to establish malaria border health facilities for Testing, Treating and Tracking (T3). The Mozambique South Africa Swaziland (MOSASWA) cross-border initiative focuses on helping countries to set up mobile clinics along the borders of these three countries [3], however, since Eswatini is a recipient of E-8 funds for the same purpose, the country reprogrammed its budget to focus on IRS, Entomological Surveillance, and Information Education Communication (IEC) [14]. Despite the presence of these mobile clinics along the border, Eswatini still had cases along the border, both autochthonous as well as imported in the study period.
Indeed, community involvement plays an important role in efforts to achieve malaria elimination as the success of interventions, including indoor residual spraying (IRS) and community case management, are effective only if they are accessible, acceptable, and properly used within communities. Many of the challenges to malaria elimination are site-specific and require a more tailored approach to effectively target the remaining malaria foci of transmission and populations at higher risk [34]. Eswatini’s NMP used community engagement platforms, stakeholder meetings, community radio stations, song and dance, roadshows, community drama, as well as home visits to involve communities in information-sharing and collaborative capacity building that sensitized communities on the elimination agenda [35].
Accurate laboratory diagnosis is essential, especially with the adoption of the T3 initiative. False-negative results can lead to untreated malaria and potentially severe consequences, including death. Surveillance systems need to capture true malaria cases for informed interventions. The WHO ‘A Framework for Malaria Elimination’ recommends in the monitoring and evaluation that a percentage of microscopy results be cross-checked by a national reference laboratory for 100% of positive results and 10% of negative results [22]. This study observed that most malaria cases were confirmed using RDT in all health care facilities, while mission/NGO-owned facilities had a higher proportion of cases confirmed by microscope. Even though Eswatini has National Quality Assurance Guidelines for Malaria Diagnosis [34] in place, the NMP has not been routinely implemented, and data was not updated in the ACD database for the samples that were checked for quality assurance. The NMP further stated that it was understaffed and lacked the capacity for routine implementation. Eswatini needs to emphasize the implementation of its guidelines by assessing the epidemiological, operational and financial situation of the malaria programme as recommended by the WHO [22] if it is to attain elimination in the future.
Adherence to the National Malaria Diagnosis and Treatment Guidelines is critical if malaria elimination is to be achieved. Almost all (85%) of the confirmed malaria cases in Eswatini were uncomplicated. However, only a little over a half (58.4%) were treated with AL + primaquine, while only 46.9% of severe malaria cases were treated with artesunate. In contradiction with recommendations in the national diagnosis and treatment guidelines, some cases of uncomplicated malaria were treated with quinine and artesunate, while some patients with severe malaria were treated with AL. Mistreatment of malaria cases could result in worsening of the patient’s health status or even death. Non-adherence to national guidelines for malaria treatment has been reported in other African countries such as Uganda [36], Nigeria [36], and Tanzania [37], but none of these countries is at the frontline of malaria elimination, unlike Eswatini. Several factors have been cited for the flouting of national guidelines by clinic staff, including delay in producing laboratory results [36, 38], inadequate supplies of the recommended drugs, and inadequate training of the prescribers [39]. It is therefore crucial for Eswatini to conduct an in-depth evaluation of the possible factors for the non-adherence of national guidelines to generate information to improve case management to achieve malaria elimination.
There are limitations in this study considering this was a retrospective study using secondary data for analysis. Since this data was already entered in the database, there was a possibility of missing data and/or wrong entry in some of the records. Health facility data has the potential for under-reporting malaria cases as a considerable proportion of people may not have presented at the health facilities due to factors such as accessibility. Furthermore, unavailable (missing) data on the mobile population and labour force such as case demographics, reasons for travelling and length of stay when travelled, made it impossible to present data on mobile populations and labour force. Also, other factors may have confounded the observed results, such as the impact of malaria control activities as well as host- and mosquito-related ecological and environmental factors. This study also looked at vector control with IRS; however, for the years 2012 and 2013, there was no IRS data. The NMP explained that the missing/lost information resulted from the Programme modifying its database during the study years.
This case study has programmatic implications. IRS has in the past been successfully proven to work in Eswatini to manage cross-border transmission via the LSDI regional malaria control collaboration [6] and has for over 70 years contributed to eliminating malaria from various countries when integrated with other measures [23]. Integrated vector management (IVM) is the rational decision-making process to maximize the impact of resources allocated for vector control for long-term sustainability [40]. It might be time for Eswatini to consider an integrated approach for malaria control by adding tools such as long-lasting insecticidal nets (LLINs) [41], screening of house entry points [42] and targeted larviciding [43] along with chemoprophylaxis to their malaria control toolbox. Operational research should support such efforts towards IVM [44], which has been demonstrated in other countries including Zambia [45] and Tanzania [46, 47]. In Zambia, the interventions include IRS, LLINs, larviciding and environmental management implemented in eligible urban and rural areas [45]. In Tanzania, integrated control of urban mosquitoes in Dar es Salaam using community sanitation supplemented by larviciding was successful in managing mosquitoes [46, 47].
Furthermore, there is a need to improve entomological surveillance in Eswatini to identify and monitor malaria vectors. Despite the country’s emphasis on vector control, surprisingly little is known about the local vector species and population dynamics, the role of secondary vectors in malaria transmission and the status of insecticide resistance. Monitoring and evaluation indicators for interventions in an elimination programme for vector control calls for independent vector surveys targeting local vectors [19]. This is a challenge Eswatini still faces because its core intervention is IRS and yet there is a lack of crucial ecological data on local malaria vectors, making the emphasis of such intervention lack factual justification. Equally, implementation of resistance management strategies and alternative approaches, including natural-based interventions, will be pivotal for effective IVM and attainment of the objectives of the Stockholm Convention [40]. A review of procedures and challenges at the programme level might help to improve vector control implementation, including routine entomological surveillance in sentinel sites in the different ecological zones. Overall, the review of the malaria control effort over the past 8 years highlights the need to invest in strengthening human resources and infrastructural capacity. These include training and retaining personnel with the necessary skills, establishing laboratories, an insectary, systems for timely procurement and appropriate storage, and adherence to standard operating procedures.
The achievement of malaria elimination requires the involvement of stakeholders in strategic planning and solicitation of funds as well as implementing strategies to achieve the desired goal of malaria elimination. Through Eswatini’s continental partnerships with the African Leaders Malaria Alliance; ALMA [35], and international stakeholders such as WHO-AFRO and Roll Back Malaria (RBM) [35], the country can and must leverage on vast capital and human resource networking. For instance, through ALMA’s scorecard for accountability and action, countries track malaria data to spur action and drive progress towards the goal of ending malaria mortality and morbidity [35]. Furthermore, through a partnership with WHO-AFRO, Eswatini benefits from financial and technical support [14] as well as the opportunity to collaborate with international organizations, such as the International Centre of Insect Physiology and Ecology (icipe) [14] which provides technical support to the programme. It is, therefore, important for Eswatini to utilize such partnerships and collaborations to address challenges the challenges that hindered the country from achieving elimination.
Source link : https://malariajournal.biomedcentral.com/articles/10.1186/s12936-021-03699-x
Author :
Publish date : 2021-03-20 07:00:00
Copyright for syndicated content belongs to the linked Source.